Let's talk about: Health Costs
Subscribe here (it's free!)
Drug prices are similar to the points in “Whose Line is it Anyway?” - they’re made up. The price that is shown in the infographic (250$) is purely artificial, considering the drug maker gives a $62.50 rebate, meaning the actual cost to the drug maker is only $187.5.
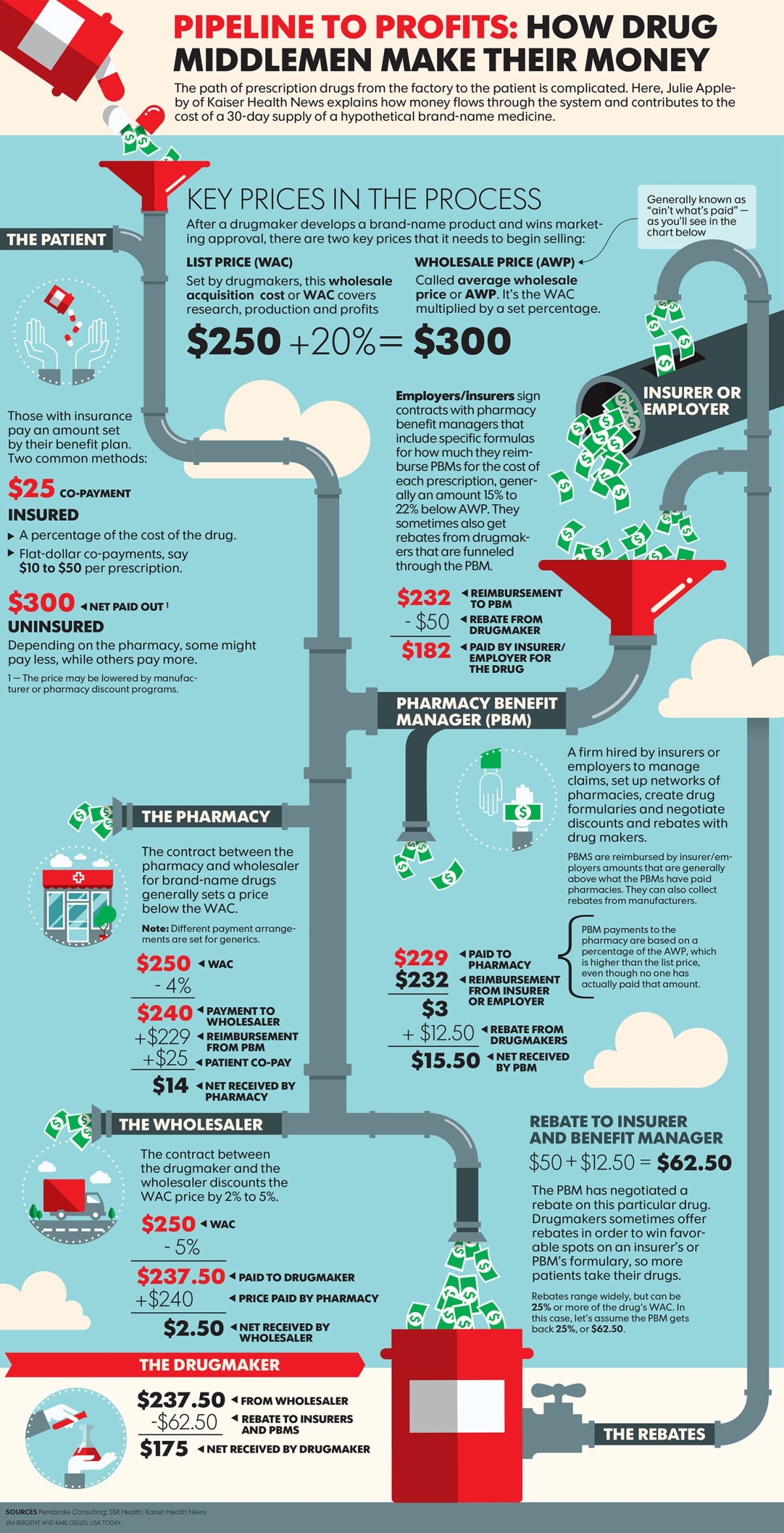
Image from Kaiser Health News shared under a CC license.
Textual description
What happens is, the company that makes the drug sets a price, let’s say 250$ (this is a “fake” price as you will see). Now, the drug is sold to a wholesaler for a certain price (237.50$ in the figure). The wholesaler then sells it to pharmacies for a profit (240$). Notice how the price dropped from 250 to 237.5? It’s because the 250 price is a lie. The actual price was always 237.50$ and 250$ was chosen to inflate the price and make it seem like the buyer is getting a great “deal”.
Now the employer pays 232$ to the pharmacy, of which the Pharmacy Benefit Managers (PBMs) pocket 3$. The pharmacy gets 229$ + another 25$ from the patient, giving the pharmacies 254$, or a 14$ profit. What’s hilarious is that the drugmaker ends up paying a 62.50$ rebate! It’s the same as someone selling you a bridge for 250$ and immediately offering you a 100$ “discount”. Assuming the drug maker never charged you the “fake” price up front, the wholesaler would be charged only 175$. Then, the wholesaler could charge the pharmacy 177.5$, meaning the pharmacy could charge 191.5$ and still get the same profit (14$) as before. This would require employers/insurers to pay just 166.5$ instead of (effectively) 182$. The 15.5$ saved by the employer comes from removing the 12.5$ “rebate” to PBMs and the 3$ profit they make. You’ll notice the 12.5$ is not really a “rebate”, but rather is profit the PBMs make.
Fixing the system
Now, how can society get to a world where the system works better than the current state? To disrupt this in a capitalistic system (meaning everyone still operates trying to make a profit) in a way that the end-customer pays lower sums, employers/insurers need to go directly to pharmacies (cut out the PBMs). Even more efficient would be cutting out the pharmacies by having employers act as “pharmacies” and buying from the wholesellers. The most “cost-efficient” approach would be for employers/insurers to start making drugs themselves. PBMs not adding anything to the process is why Hasan Minhaj focuses on them in his segment on drug pricing.
Another way would be for the employers to operate a “competing pharmacy” that sells medicines to their employees. As employers would be saving costs, they wouldn’t need to make as much profits as these pharmacies for this to be a good decision financially for them. This may be what Amazon is doing with Pillpack.
What’s preventing these fixes? I would guess lobbying by pharmaceutical companies (and other players in the chain) and/or ensuring that the market is not entirely free (no competition from abroad allowed, no freedom for drug makers to make deals directly with employers/insurers, etc.).
Does stuff work the same way in healthcare?
I would guess yes. Except now there are three sources of payments - your premiums (monthly payment to your insurance plan), your co-pays/deductibles and your insurance’s payment. These are all decided by your insurance, so maybe if you could pay your hospital directly these costs could be lower. However, the hospital/care provider may need to charge you more than just the costs they incurred to care for you, in order to account for those who don’t have insurance. So, insurance plans may seem better (there are lots of debates on this). Some of this is covered by Adam Conover in Adam Ruins Everything.
Things I still don’t understand
Why is the 300$ number even mentioned in the infographic?
Why do uninsured people pay 300$? The general idea for uninsured people paying more is to offset the costs of other people who are uninsured who won’t end up paying. However, unliked healthcare, I would assume to get a drug, you pay first and get the drug only after payment has been made.